SHOULDER STABILISATION SURGERY
MELBOURNE
SHOULDER JOINT ANATOMY
What are the joints, muscles and ligaments in your shoulder?
The shoulder is made up of three bones:
(1) The Scapula (shoulder blade), (2) Clavicle (collarbone) and; (3) Humerus (upper arm bone)
The shoulder joint is formed where the humerus (upper arm bone) fits into the scapula (shoulder blade), like a ball and socket.
Other important shoulder bones include:
The acromion – The bony projection off the scapula.
The clavicle (collarbone) – This meets the acromion in the acromioclavicular joint.
The coracoid process – The hook-like bony projection from the scapula.
The shoulder has several other important structures including:
The bursa – A small sac of fluid that cushions and protects the tendons of the rotator cuff.
The rotator cuff – A collection of muscles and tendons that surround the shoulder, giving it support and allowing a wide range of motion.
The labrum – A cuff of cartilage that forms a lip for the ball-like head of the humerus to fit into the socket.
The humerus fits relatively loosely into the shoulder joint, allowing the shoulder a wide range of motion.
Shoulder Anatomy
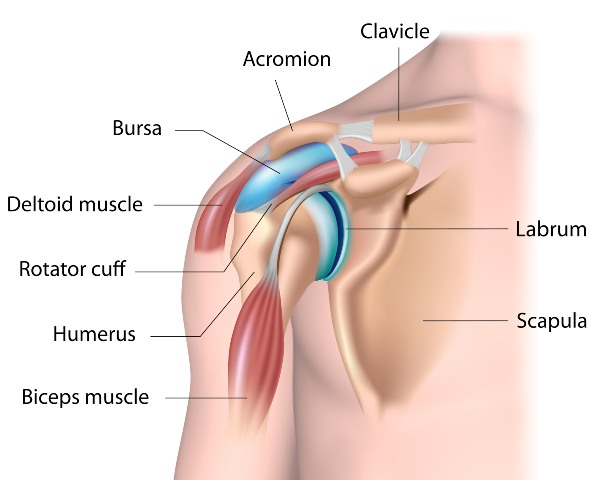
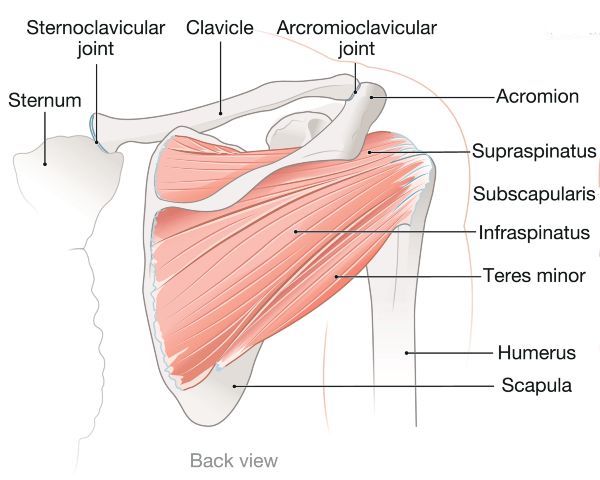
Figure 1
SHOULDER STABILISATION SURGERY MELBOURNE
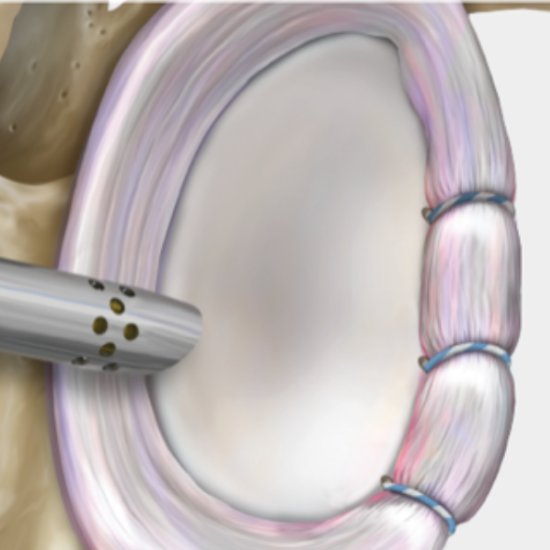 Doctor Pullen will examine your shoulder under anesthesia (usually via arthroscopic surgery) to fully assess the condition of the labrum and rotator cuff tendons to identify the extent and direction of the instability.
Doctor Pullen will examine your shoulder under anesthesia (usually via arthroscopic surgery) to fully assess the condition of the labrum and rotator cuff tendons to identify the extent and direction of the instability.
In some patients the degree of looseness is mild and the shoulder may be stabilised by arthroscopic techniques.
Severe shoulder instability may require open surgery where an incision is made over the shoulder and the muscles moved aside in order to gain access to the shoulder joint.
The injured structures are then either repaired, reattached or tightened.
The repair is usually performed with sutures attached to metal or plastic anchors.
These anchors are inserted into the bone and hold the sutures that are used to reattach or tighten the ligaments. These anchors stay in the bone permanently.
The surgery usually takes around two hours and has a 6 month rehabilitation and recovery period.
Image – Repair of the glenoid labrum using suture anchors.
POTENTIAL COMPLICATIONS
The surgery complications which may occur after shoulder stabilisation surgery include:
- Shoulder stiffness and restricted movement
- Infection
- Numbness or tingling around the shoulder
- Recurrent tendon tear.
Dr Pullen will discuss with you in detail the potential complications and risks in relation to the surgery.
Proud member of Royal Australasian College of Surgeons and Australian Orthopaedic Association.


Shoulder Stabilisation Surgery Melbourne
Dr Pullen treats patients from all over Victoria in relation to shoulder injuries. He consults with patients at the following practice locations in Melbourne including East Melbourne and Ringwood.


 Shoulder instability describes a feeling of looseness in the shoulder joint that may result in pain, partial or complete shoulder dislocation
Shoulder instability describes a feeling of looseness in the shoulder joint that may result in pain, partial or complete shoulder dislocation